Introduction to Bronchiolitis
Bronchiolitis is a prevalent lower respiratory tract infection characterized by inflammation and obstruction of the small airways in the lungs, specifically the bronchioles. It is a significant cause of morbidity in infants and young children worldwide, particularly during the winter months in temperate climates. The condition is primarily caused by viral infections, with Respiratory Syncytial Virus (RSV) being the most common culprit. However, other viruses such as human metapneumovirus, influenza, and parainfluenza viruses can also lead to bronchiolitis.
Epidemiology and Burden
Bronchiolitis affects infants and young children under the age of 2 years, with peak incidence occurring between 3 to 6 months of age. In developed countries, it is one of the leading causes of hospitalization in infants, especially those born prematurely or with underlying medical conditions. The incidence varies seasonally, with outbreaks typically occurring during the colder months when respiratory viruses are more prevalent.
Etiology and Pathophysiology
Causal Agents
Respiratory viruses are the primary cause of bronchiolitis, with RSV responsible for a significant majority of cases. RSV is a negative-sense, single-stranded RNA virus belonging to the Paramyxoviridae family. It spreads via respiratory droplets and direct contact with contaminated surfaces. Other viruses implicated in bronchiolitis include human metapneumovirus, influenza viruses (types A and B), parainfluenza viruses, adenovirus, and rhinovirus.
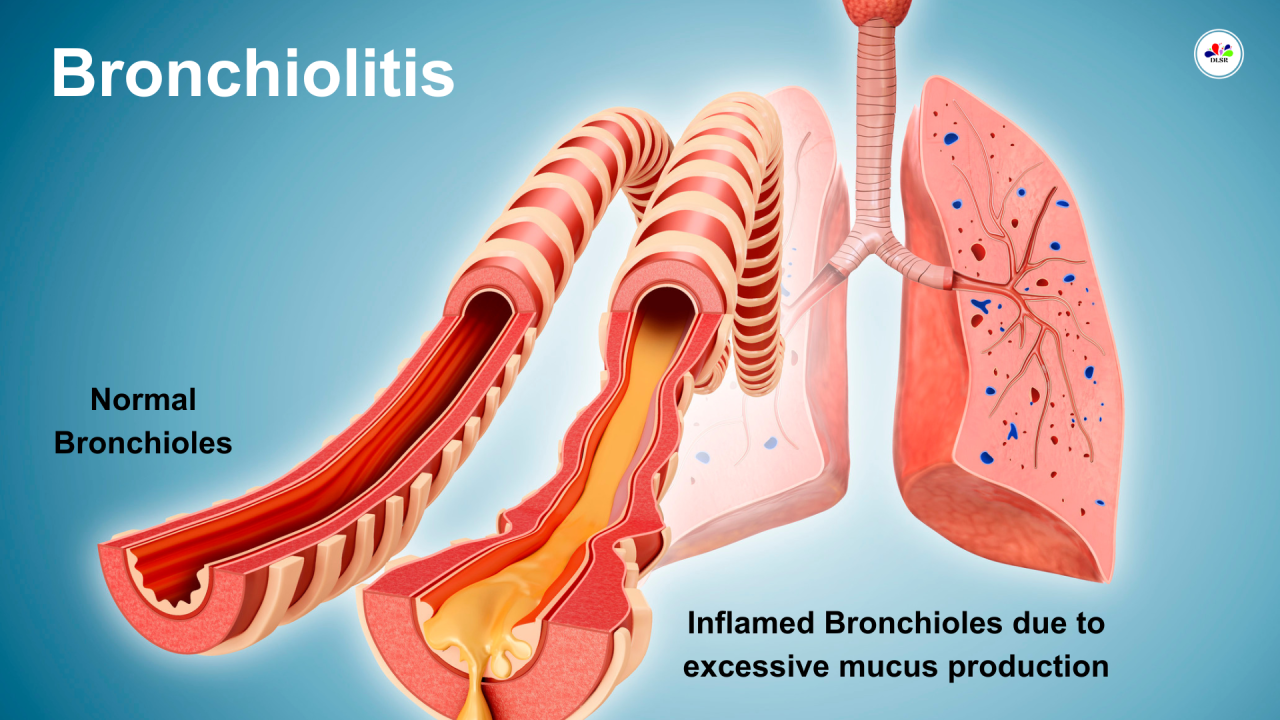
Pathophysiological Mechanisms
Bronchiolitis begins with viral replication in the upper respiratory tract epithelium. The virus then spreads to the lower respiratory tract, infecting the bronchioles. This infection triggers an inflammatory response characterized by infiltration of inflammatory cells (neutrophils, lymphocytes) into the bronchiolar walls. As a result, there is edema and increased mucus production, leading to narrowing of the bronchiolar lumen. The combination of inflammation, mucus plugging, and bronchoconstriction results in airway obstruction and impaired gas exchange, manifesting clinically as respiratory distress.
Clinical Presentation
Signs and Symptoms
The clinical presentation of bronchiolitis can vary from mild respiratory symptoms to severe respiratory distress requiring intensive care. Common signs and symptoms include:
- Cough: Initially dry, may progress to productive cough with clear or white sputum.
- Wheezing: High-pitched, musical sounds heard primarily during expiration.
- Tachypnea: Increased respiratory rate (> 60 breaths per minute in infants).
- Nasal Flaring and Retractions: Signs of increased work of breathing.
- Fever: Often low-grade, but can be higher in some cases.
- Decreased Feeding and Lethargy: Due to respiratory distress and increased energy expenditure.
Severity Grading
Bronchiolitis severity is typically categorized based on clinical findings:
- Mild: Symptoms are mild, with minimal respiratory distress.
- Moderate: Increased work of breathing but able to maintain oral hydration.
- Severe: Marked respiratory distress, often requiring supplemental oxygen and hospitalization.
- Critical: Respiratory failure necessitating mechanical ventilation.
Diagnosis and Differential Diagnosis
Diagnostic Approach
The diagnosis of bronchiolitis is primarily clinical, based on history and physical examination findings. Key diagnostic features include age (typically < 2 years), viral prodrome (rhinorrhea, congestion), and characteristic respiratory signs (wheezing, crackles). Diagnostic testing, such as nasopharyngeal swabs for viral PCR, is not routinely recommended in clinical practice but may be considered in severe cases or outbreaks to guide infection control measures.
Differential Diagnosis
Several conditions can mimic bronchiolitis, including:
- Asthma: Especially in older children presenting with recurrent wheezing.
- Pneumonia: Bacterial or viral pneumonia may present similarly but typically have focal findings on chest examination and infiltrates on chest imaging.
- Foreign Body Aspiration: Consider in children with sudden onset of symptoms and unilateral wheezing.
Risk Factors
Predisposing Factors
Certain factors increase the risk of severe bronchiolitis:
- Age: Infants younger than 6 months are at higher risk due to immature immune systems and smaller airway size.
- Prematurity: Preterm infants with underdeveloped lungs are more susceptible.
- Chronic Lung Disease: Such as bronchopulmonary dysplasia.
- Congenital Heart Disease: Impairs respiratory reserve and increases susceptibility to viral infections.
- Immunocompromised States: Including HIV infection or chemotherapy.
Environmental Factors
Exposure to environmental tobacco smoke, crowded living conditions, and lack of breastfeeding can also increase the risk of severe bronchiolitis.
Management and Treatment
Supportive Care
The cornerstone of bronchiolitis management is supportive care:
- Hydration: Adequate oral or intravenous fluids to prevent dehydration.
- Oxygen Therapy: Supplemental oxygen to maintain adequate oxygenation.
- Nutritional Support: Ensuring adequate calorie intake despite decreased oral intake.
Pharmacological Interventions
- Bronchodilators: Generally not recommended as routine therapy due to lack of proven benefit in bronchiolitis. May be considered in select cases with significant wheezing.
- Corticosteroids: Not recommended routinely due to lack of consistent benefit and potential adverse effects.
- Antiviral Therapy: Limited role, primarily reserved for severe cases or high-risk infants.
Respiratory Support
- Mechanical Ventilation: Required in severe cases with respiratory failure.
- Continuous Positive Airway Pressure (CPAP): Non-invasive ventilation modality used to support breathing and improve oxygenation.
Hospitalization Criteria
Infants with bronchiolitis may require hospitalization based on:
- Clinical Severity: Moderate to severe respiratory distress.
- Age: Young age (< 3 months) or prematurity.
- Underlying Medical Conditions: Chronic lung disease, congenital heart disease.
- Social Factors: Inadequate home support or inability to provide adequate oral intake.
Prevention Strategies
Vaccination
No specific vaccine against RSV is currently available for routine use, although passive immunoprophylaxis with palivizumab (monoclonal antibody) is recommended for certain high-risk infants during RSV season.
Hygiene Measures
- Hand Hygiene: Regular handwashing, especially before handling infants.
- Respiratory Etiquette: Covering mouth and nose when coughing or sneezing.
- Avoidance of Smoke Exposure: Particularly in households with infants and young children.
Complications
Respiratory Complications
- Atelectasis: Collapse of lung tissue due to mucus plugging or airway obstruction.
- Respiratory Failure: Inability to maintain adequate gas exchange, requiring mechanical ventilation.
- Pneumothorax: Rare complication associated with positive pressure ventilation.
Long-Term Respiratory Effects
Children with severe bronchiolitis may have an increased risk of recurrent wheezing and asthma later in childhood, although the exact mechanisms are not fully understood.
Economic and Social Impacts
Healthcare Utilization
Bronchiolitis places a significant burden on healthcare systems due to hospital admissions, emergency department visits, and outpatient clinic visits during peak respiratory virus seasons.
Impact on Families
- Work Absenteeism: Parents may miss work due to caring for sick children or hospitalization.
- Psychological Stress: Anxiety and emotional strain associated with caring for a sick infant, especially in severe cases requiring intensive care.
Research and Future Directions
Current Research Trends
- Vaccine Development: Efforts to develop an effective RSV vaccine for broader population use.
- Genetic Susceptibility: Understanding genetic factors influencing susceptibility to severe bronchiolitis.
- Antiviral Therapies: Investigating novel antiviral agents targeting respiratory viruses.
Emerging Epidemiological Patterns
- Changing Viral Strains: Evolution of viral strains and their impact on disease severity and vaccine efficacy.
- Global Impact: Bronchiolitis burden in developing countries and strategies for resource-limited settings.
Conclusion
Bronchiolitis is a common respiratory illness affecting infants and young children worldwide, characterized by inflammation and obstruction of the bronchioles due to viral infections, primarily RSV. Management is primarily supportive, focusing on hydration, oxygenation, and respiratory support as needed. Prevention strategies include vaccination where available, hygiene measures, and avoidance of smoke exposure. While most cases resolve without complications, severe bronchiolitis can lead to respiratory failure and long-term respiratory sequelae. Ongoing research aims to improve prevention strategies, understand disease mechanisms, and develop targeted therapies. By enhancing our understanding of bronchiolitis, healthcare providers can optimize management and reduce the overall burden of this significant pediatric respiratory condition.